Published online Feb 26, 2015. doi: 10.13105/wjma.v3.i1.26
Peer-review started: April 12, 2014
First decision: May 1, 2014
Revised: December 18, 2014
Accepted: December 29, 2014
Article in press: December 31, 2014
Published online: February 26, 2015
Processing time: 283 Days and 9.9 Hours
AIM: To determine whether institutional laparoscopy cholecystectomy (LC) volume affects rates of mortality, conversion to open surgery, bile leakage and bile duct injury (BDI).
METHODS: Eligible studies were prospective or retrospective cohort studies that provided data on outcomes from consecutive LC procedures in single institutions. Relevant outcomes were mortality, conversion to open surgery, bile leakage and BDI. We performed a Medline search and extracted data. A regression analysis using generalized estimating equations were used to determine the influence of annual institutional LC caseload on outcomes. A sensitivity analysis was performed including only those studies that were published after 1995.
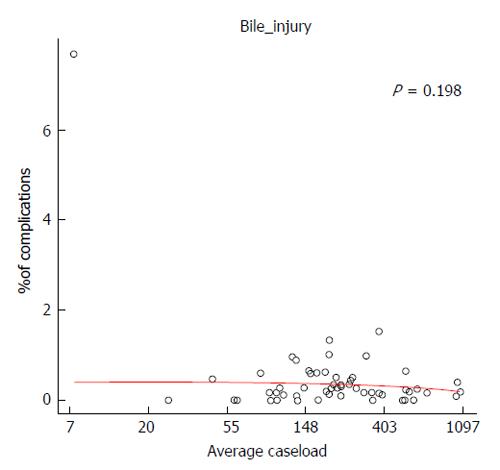
RESULTS: Seventy-three cohorts (127404 LC procedures) were included. Average complication rates were 0.06% for mortality, 3.23% for conversion, 0.44% for bile leakage and 0.28% for bile duct injury. Annual institutional caseload did not influence rates of mortality (P = 0.142), bile leakage (P = 0.111) or bile duct injury (P = 0.198) although increasing caseload was associated with reduced incidence of conversion (P = 0.019). Results from the sensitivity analyses were similar.
CONCLUSION: Institutional volume is a determinant of LC complications. It is unclear whether volume is directly linked to complication rates or whether it is an index for protocolised care.
Core tip: We performed a meta-analysis to determine whether institutional laparoscopy cholecystectomy (LC) volume affects rates of mortality, conversion to open surgery, bile leakage and bile duct injury. Annual institutional caseload did not influence rates of mortality (P = 0.142), bile leakage (P = 0.111) or bile duct injury (P = 0.198) although increasing caseload was associated with reduced incidence of conversion (P = 0.019). Our results suggest that institutional LC volume may be a determinant of LC complications. It is unclear whether institutional LC volume is directly linked to complication rates or whether its influence is a surrogate for improved quality of care.
- Citation: Murray M, Healy DA, Ferguson J, Bashar K, McHugh S, Clarke Moloney M, Walsh SR. Effect of institutional volume on laparoscopic cholecystectomy outcomes: Systematic review and meta-analysis. World J Meta-Anal 2015; 3(1): 26-35
- URL: https://www.wjgnet.com/2308-3840/full/v3/i1/26.htm
- DOI: https://dx.doi.org/10.13105/wjma.v3.i1.26
Laparoscopic cholecystectomy (LC) is one of the most commonly performed operations-close to 400000 procedures are performed annually in non-federal community hospitals in the United States[1] and around 50000 procedures are performed annually in the United Kingdom[2]. LC is preferred over open cholecystectomy as it leads to a shorter hospital stay and a quicker recovery[3]. However, there are risks of serious complications with LC such as biliary leaks (0.4%-1%)[2,4], bile duct injury (BDI) (0.2%-0.3%)[3,5] and mortality (0.1%-0.4%)[3,5]. Conversion rates vary from about 15%-5%[5].
An expanding body of evidence suggests that outcomes in a variety of conditions are improved when patients are managed in high-volume centres or by high-volume healthcare providers[6]. High-volume centres dramatically improve the management of pancreatic cancer (≥ 20 cases per year), oesophageal cancer (≥ 30 cases per year), paediatric cardiac conditions (≥ 300 cases per year), unruptured abdominal aortic aneurysms (AAA) (≥ 36 cases per year) and acquired immune deficiency syndrome (≥ 100 cases per year)[6]. Similarly, high-volume surgeons or physicians dramatically improve the management of pancreatic cancer (10-42 cases per year), ruptured AAAs (≥ 10 cases per year), paediatric cardiac conditions (≥ 75 cases per year), colorectal cancer (≥ 22 cases per year), carotid endarterectomy (≥ 30 cases per year) and coronary artery bypass grafting (≥ 150 cases per year)[6]. In contrast, no proven volume-outcome relationships exist for conditions such as diabetes, cystic fibrosis, rheumatoid arthritis, appendicitis and hernias[7,8].
Recently, data have emerged confirming that high-volume surgeons improve outcomes following LC[2,4,5,9-12]. Giger et al[5] found improved results with surgeons who performed > 100 LCs per year, Nuzzo et al[10] found improved results with surgical teams who performed > 450 LCs in three years, Csikesz et al[11] found improved results with surgeons who performed > 15 LCs per year and McMahon et al[12] found improved results for surgeons who had performed more than 200 cases. Andrews et al[2] and Hobbs et al[4] did not specify thresholds although they identified significantly reduced complications with increasing surgeon volume. However, it is unclear whether a volume-outcome relationship exists for LC at institutional level. If such an institutional relationship can be proven and understood, the creation of high-volume LC centres may become a priority. Therefore we performed a systematic review and meta-analysis focusing on institutional volume/outcome relationships for LC. The aim was to determine whether institutional LC volume affects rates of mortality, conversion to open surgery, bile leakage and bile duct injury.
This systematic review was performed in accordance with the PRISMA guidelines[13]. These guidelines are an evidence-based set of items that aim to enhance methodological and reporting clarity.
The Medline electronic database was searched from 1st January 1990 to 9th April 2014 using the free text “laparoscopic cholecystectomy”.
Eligible studies were prospective or retrospective cohort studies that provided details on outcomes from consecutive LC procedures in single institutions. The relevant outcomes were the incidences of conversion to open surgery, bile leakage, BDI or mortality. The definitions and timeframes of these outcomes were those specified in retrieved manuscripts. There were no limitations on cohort sizes or on recruitment dates of studies. Studies reporting combined results from multiple centres were eligible provided that data were provided separately for individual centres. Studies were excluded if results did not allow the calculation of institutional complication rates. This lead to the exclusion of studies that reported on selected LCs rather than all consecutive LCs and studies that did not specify study start and finish dates. Case reports, narrative reviews and non-English language studies were also excluded.
One author (Murray M) identified eligible studies. Firstly, titles and abstracts were screened. Full-text manuscripts of potentially relevant studies were examined to finalise eligibility. Uncertainties regarding eligibility were discussed with a second author (Healy DA). For each included study, the following data were extracted independently by two authors (Murray M and Healy DA): author, publication date, study design, the institution’s name, start and finish dates, duration, number of LCs, number of mortalities, number of conversions to open surgery, number of bile leaks and the number of cases of BDI. Percentage complication rates were calculated for each outcome. Disagreements regarding data extraction were resolved by discussion with a third author (Walsh SR). Data were entered into a computerised spreadsheet for analysis.
All analyses were designed and performed by a biomedical statistician (JF). Scatterplots were used to summarise the relationships between numbers of LC procedures per year and percentage complication rates. Regression analyses were performed using generalized estimating equations. The generalized estimation equations were fit using a variance structure based on the binomial distribution. The response was the percentage of complications out of all procedures performed. A robust variance was used to account for extra variance around the regression line because of center specific effects. The function “gee” in the statistical language R was used. A sensitivity analysis was performed that was limited to studies that were published after 1995. This time point was chosen with the aim of eliminating the effects of learning curves and improvements in perioperative care. Significance was set at 5%.
The authors state that all statistical analyses were designed and performed by a biomedical statistician. A statement to this effect is included in the methods section.
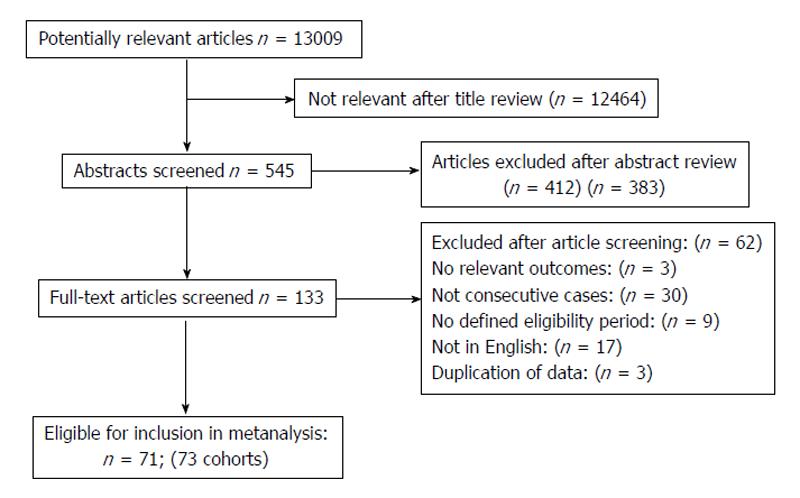
Figure 1 summarises the results of the search. 13009 citations were identified and 12876 were excluded based on titles and abstracts. 133 full text manuscripts were retrieved and 71 articles (corresponding to 73 cohorts) were finally eligible for inclusion.
Table 1 provides a summary of the 73 eligible cohorts[14-84]. Most were retrospective and some were prospective cohorts. Study recruitment periods varied from 1990 to 2013. The total number of LC procedures was 127404.
| Ref. | Publication | Study duration | Design | Total LC | Average annual | Mortality | Percentage | Conversion to open | Percentage | Bile leak | Percentage bile | Bile duct injury | Percentage bile |
| year | in months | number | LC number | incidence | mortality rate (%) | surgery incidence | conversion rate (%) | incidence | leak rate (%) | incidence | duct injury rate (%) | ||
| Szego et al[14] | 1991 | 6 | Retrospective | 31 | 62.00 | 0 | 0.00 | 2 | 6.45 | 0 | 0 | 0 | 0 |
| Bailey et al[15] | 1991 | 16 | Prospective | 375 | 281.25 | 1 | 0.27 | 20 | 5.33 | 1 | 0.27 | 1 | 0 |
| Peters et al[16] | 1991 | 6 | Prospective | 100 | 200.00 | 0 | 0.00 | 4 | 4.00 | 2 | 2 | 1 | 1 |
| Rees et al[17] | 1992 | 12 | Retrospective | 155 | 155.00 | N/A | N/A | 8 | 5.16 | 2 | 1.29 | 1 | 1 |
| Huang et al[18] | 1992 | 11 | Retrospective | 200 | 218.18 | N/A | N/A | N/A | N/A | 1 | 0.5 | 1 | 1 |
| Davis et al[19] | 1992 | 24 | Retrospective | 622 | 311.00 | N/A | N/A | 26 | 4.18 | N/A | N/A | 1 | 0 |
| Fielding et al[20] | 1992 | 12 | Retrospective | 220 | 220.00 | N/A | N/A | 8 | 3.64 | 2 | 0.91 | N/A | N/A |
| Soper et al[21] | 1992 | 21 | Prospective | 600 | 342.80 | 0 | 0.00 | 18 | 3.00 | N/A | N/A | 1 | 0 |
| Périssat et al[22] | 1992 | 32 | Retrospective | 700 | 262.50 | 1 | 0.14 | 41 | 5.86 | N/A | N/A | 3 | 0 |
| Troidl et al[23] | 1992 | 14.5 | Prospective | 400 | 331.00 | 2 | 0.50 | 20 | 5.00 | 3 | 0.75 | N/A | N/A |
| Rubio et al[24] | 1993 | 31 | Retrospective | 500 | 193.55 | N/A | N/A | 4 | 0.80 | 1 | 0.2 | 1 | 0 |
| Huang et al[25] | 1993 | 18 | Retrospective | 350 | 233.33 | 0 | 0.00 | 6 | 1.71 | 4 | 1.14 | 1 | 0 |
| Cox et al[26] | 1994 | 24 | Prospective | 410 | 205.00 | N/A | N/A | N/A | N/A | N/A | N/A | 1 | 0 |
| Williams et al[27] | 1994 | 27 | Retrospective | 600 | 266.67 | 1 | 0.17 | 24 | 4.00 | N/A | N/A | 3 | 1 |
| Cappuccino et al[28] | 1994 | 14 | Retrospective | 563 | 482.57 | 0 | 0.00 | 5 | 0.89 | N/A | N/A | N/A | N/A |
| Bonatsos et al[29] | 1995 | 41 | Retrospective | 1788 | 523.32 | 0 | 0.00 | 45 | 2.52 | 19 | 1.06 | 0 | 0 |
| Newman et al[30] | 1995 | 36 | Retrospective | 1525 | 508.33 | 4 | 0.26 | 34 | 2.23 | 0 | 0 | 0 | 0 |
| Chen et al[31] | 1996 | 42 | Retrospective | 2428 | 693.71 | 1 | 0.04 | N/A | N/A | 1 | 0.04 | 4 | 0 |
| Bond et al[32] | 1996 | 36 | Retrospective | 534 | 178.00 | 2 | 0.37 | N/A | N/A | N/A | N/A | N/A | N/A |
| Sartori et al[33] | 1996 | 14 | Retrospective | 322 | 276.00 | 0 | 0.00 | N/A | N/A | N/A | N/A | N/A | N/A |
| Rather et al[34] | 1997 | 24 | Retrospective | 340 | 170.00 | 0 | 0.00 | 26 | 7.65 | 6 | 1.76 | 2 | 1 |
| Jan et al[35] | 1997 | 60 | Retrospective | 1115 | 223.00 | N/A | N/A | N/A | N/A | 4 | 0.36 | 3 | 0 |
| Ahmad et al[36] | 1997 | 45 | Retrospective | 1300 | 346.67 | 0 | 0.00 | 40 | 3.08 | 6 | 0.46 | 0 | 0 |
| Kok et al[37] | 1998 | 58 | Prospective | 220 | 45.52 | 1 | 0.45 | 9 | 4.09 | N/A | N/A | 1 | 0 |
| Targarona et al[38] | 1998 | 61 | Retrospective | 1630 | 320.66 | N/A | N/A | 109 | 6.69 | N/A | N/A | 16 | 1 |
| Kurauchi et al[39] | 1998 | 32 | Retrospective | 1408 | 528.00 | 1 | 0.07 | 89 | 6.32 | N/A | N/A | 9 | 1 |
| Jones-Monahan et al[40] | 1998 | 60 | Retrospective | 2654 | 530.80 | N/A | N/A | N/A | N/A | 1 | 0.04 | 6 | 0 |
| Matthews et al[41] | 1999 | 53 | Retrospective | 1025 | 232.08 | 3 | 0.29 | 27 | 2.63 | 2 | 0.2 | 1 | 0 |
| Calvete et al[42] | 2000 | 72 | Prospective | 784 | 130.67 | 0 | 0.00 | 4 | 0.51 | 4 | 0.51 | 7 | 1 |
| Patel et al[43] | 2000 | 38 | Prospective | 135 | 42.63 | 0 | 0.00 | 7 | 5.19 | 2 | 1.48 | N/A | N/A |
| Sikora et al[44] | 2001 | 72 | Retrospective | 1200 | 200.00 | N/A | N/A | N/A | N/A | N/A | N/A | 16 | 1 |
| Lichten et al[45] | 2001 | 12 | Retrospective | 300 | 300.00 | N/A | N/A | 17 | 5.67 | N/A | N/A | N/A | N/A |
| Miroshnik et al[46] | 2002 | 110 | Retrospective | 1216 | 132.65 | N/A | N/A | 90 | 7.40 | 7 | 0.58 | 1 | 0 |
| Hasaniah et al[47] | 2002 | 84 | Retrospective | 2750 | 392.86 | 0 | 0.00 | 127 | 4.62 | 11 | 0.4 | 3 | 0 |
| Fathy et al[48] | 2003 | 93 | Retrospective | 2000 | 258.06 | N/A | N/A | 147 | 7.35 | 11 | 0.55 | 7 | 0 |
| Duca et al[49] | 2003 | 108 | Retrospective | 9542 | 1060.22 | 10 | 0.10 | 184 | 1.93 | 54 | 0.57 | 17 | 0 |
| Mahatharadol et al[50] | 2004 | 116 | Retrospective | 1522 | 157.45 | N/A | N/A | N/A | N/A | N/A | N/A | 9 | 1 |
| Daradkeh et al[51] | 2005 | 108 | Retrospective | 1208 | 134.22 | 0 | 0.00 | 32 | 2.65 | N/A | N/A | 0 | 0 |
| Diamantis et al[52] | 2005 | 132 | Retrospective | 2079 | 189.00 | N/A | N/A | N/A | N/A | N/A | N/A | 13 | 1 |
| Söderlund et al[53] | 2005 | 50 | Prospective | 1568 | 376.32 | N/A | N/A | N/A | N/A | 23 | 1.47 | 24 | 2 |
| Baird[54] | 2005 | 16 | Prospective | 782 | 586.50 | 1 | 0.13 | 18 | 2.30 | N/A | N/A | 0 | 0 |
| Vagenas et al[55] | 2006 | 156 | Retrospective | 1220 | 93.85 | 0 | 0.00 | 23 | 1.89 | 3 | 0.25 | 2 | 0 |
| Tan et al[56] | 2006 | 9 | Prospective | 202 | 269.33 | N/A | N/A | 14 | 6.93 | 3 | 1.49 | 1 | 0 |
| Mufti et al[57] | 2007 | 12 | Retrospective | 60 | 60.00 | 0 | 0.00 | 3 | 5.00 | 1 | 1.67 | 0 | 0 |
| Brekalo et al[58] | 2007 | 120 | Retrospective | 952 | 95.20 | 1 | 0.11 | 32 | 3.36 | N/A | N/A | 0 | 0 |
| Marakis et al[59] | 2007 | 144 | Retrospective | 1225 | 102.08 | N/A | N/A | 91 | 7.43 | 1 | 0.08 | 2 | 0 |
| Herve et al[60] | 2007 | 120 | Retrospective | 1255 | 125.50 | 3 | 0.24 | 25 | 1.99 | N/A | N/A | 12 | 1 |
| Brekalo et al[58] | 2007 | 120 | Retrospective | 1066 | 106.60 | 1 | 0.09 | N/A | N/A | 43 | 4.03 | 3 | 0 |
| Shrestha et al[61] | 2007 | 21 | Prospective | 140 | 80.00 | N/A | N/A | 13 | 9.29 | N/A | N/A | N/A | N/A |
| Tantia et al[62] | 2008 | 156 | Retrospective | 13305 | 1023.46 | 0 | 0.00 | 8 | 0.06 | 10 | 0.08 | 52 | 0 |
| Priego et al[63] | 2009 | 204 | Retrospective | 3933 | 231.35 | 5 | 0.13 | 331 | 8.42 | 17 | 0.43 | 13 | 0 |
| Avgerinos et al[64] | 2009 | 72 | Prospective | 1046 | 174.33 | N/A | N/A | 27 | 2.58 | 5 | 0.48 | 0 | 0 |
| Clegg-Lamptey et al[65] | 2010 | 24 | Prospective | 52 | 26.00 | 0 | 0.00 | 1 | 1.92 | 1 | 1.92 | 0 | 0 |
| Al-Kubati et al[66] | 2010 | 48 | Retrospective | 336 | 84.00 | 0 | 0.00 | 43 | 12.80 | 3 | 0.89 | 2 | 1 |
| Ying et al[67] | 2010 | 144 | Retrospective | 2400 | 200.00 | 2 | 0.08 | 11 | 0.46 | 7 | 0.29 | 3 | 0 |
| Zha et al[68] | 2010 | 156 | Prospective | 13000 | 1000.00 | N/A | N/A | N/A | N/A | N/A | N/A | 11 | 0 |
| Wichmann et al[69] | 2010 | 18 | Prospective | 140 | 93.33 | N/A | N/A | 11 | 7.86 | 3 | 2.14 | N/A | N/A |
| Wichmann et al[69] | 2010 | 18 | Prospective | 219 | 146.00 | N/A | N/A | 18 | 8.22 | 2 | 0.91 | N/A | N/A |
| Kanakala et al[70] | 2011 | 120 | Retrospective | 2117 | 211.70 | 10 | 0.47 | 133 | 6.28 | 31 | 1.46 | 7 | 0 |
| Al-Mulhim et al[71] | 2011 | 36 | Prospective | 968 | 322.67 | N/A | N/A | 5 | 0.52 | 3 | 0.31 | N/A | N/A |
| Halilovic et al[72] | 2011 | 12 | Prospective | 293 | 293.00 | 1 | 0.34 | 8 | 2.73 | N/A | N/A | N/A | N/A |
| Hasbahceci et al[73] | 2012 | 129 | Retrospective | 1557 | 144.84 | 2 | 0.13 | 39 | 2.50 | 10 | 0.64 | 4 | 0 |
| Bekele et al[74] | 2012 | 60 | Retrospective | 681 | 136.20 | 1 | 0.15 | 20 | 2.94 | N/A | N/A | N/A | N/A |
| Le et al[75] | 2012 | 24 | Retrospective | 3371 | 1685.50 | N/A | N/A | 86 | 2.55 | N/A | N/A | N/A | N/A |
| Afuwape et al[76] | 2012 | 20 | Retrospective | 13 | 7.80 | 0 | 0.00 | 1 | 7.69 | N/A | N/A | 1 | 8 |
| Grbas et al[77] | 2013 | 202 | Retrospective | 10317 | 612.89 | 2 | 0.02 | 220 | 2.13 | 52 | 0.5 | 25 | 0 |
| Sultan et al[78] | 2013 | 120 | Retrospective | 4434 | 443.40 | N/A | N/A | 234 | 5.28 | N/A | N/A | N/A | N/A |
| Pulvirenti et al[79] | 2013 | 120 | Retrospective | 882 | 88.20 | N/A | N/A | 51 | 5.78 | N/A | N/A | N/A | N/A |
| Dip et al[80] | 2014 | 5 | Prospective | 43 | 103.20 | 0 | 0.00 | N/A | N/A | 0 | 0 | 0 | 0 |
| Comajuncosas et al[81] | 2014 | 12 | Prospective | 276 | 276.00 | N/A | N/A | 26 | 9.42 | N/A | N/A | N/A | N/A |
| Paajanen et al[82] | 2014 | 204 | Retrospective | 1895 | 111.47 | 2 | 0.11 | 126 | 6.65 | 14 | 0.74 | 2 | 0 |
| Alvarez et al[83] | 2014 | 248 | Retrospective | 11423 | 552.73 | N/A | N/A | N/A | N/A | 5 | 0.04 | 20 | 0.18 |
| Afaneh et al[84] | 2014 | 44 | Retrospective | 1382 | 376.91 | N/A | N/A | 44 | 3.18 | N/A | N/A | 2 | 0.14 |
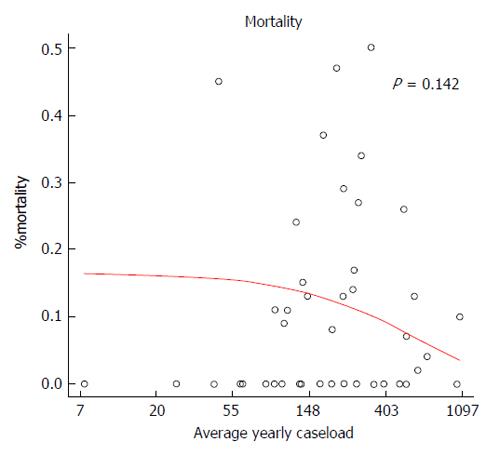
Forty-three studies (71305 patients) provided data on mortality (43 cases of mortality; average mortality was 0.06%). Figure 2 displays the relationship between average annual number of LC procedures and institutional mortality rates as percentages. There was no significant relationship between mortality and annual number of procedures (P = 0.142). When only those cohorts published after 1995 were included (32 cohorts, 64273 patients) there was no significant relationship (P = 0.168).
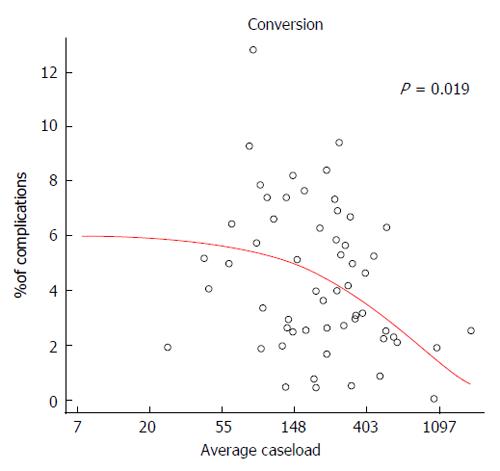
Fifty-eight studies (87840 patients) provided data on conversion rates (2835 cases of conversion; average conversion rate was 3.23%). Figure 3 displays the relationship between average annual number of LC procedures and institutional percentage conversion rates. Increasing caseload was associated with lower conversion rates (P = 0.019). When only those studies that were published after 1995 were included (43 studies, 79311 patients) the result remained significant (P = 0.019).
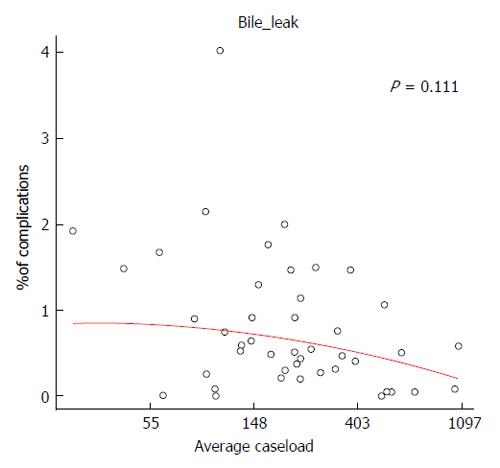
Forty-four studies (86025 patients) provided data on bile leak rates (381 cases of bile leakage; average bile leak rate was 0.44%). Figure 4 displays the relationship between average annual number of LC procedures and the institutional percentage bile leak rate. There was no significant relationship between bile leak rates and annual number of procedures (P = 0.111). When only those studies that were published after 1995 were included (33 cohorts, 80381 patients) the result was similar (P = 0.123).
Fifty-six cohorts (113526 patients) provided data on bile duct injury rates (316 cases of bile duct injury; average bile duct injury rate was 0.28%). Figure 5 displays the relationship between average annual number of LC procedures and institutional percentage bile duct injury rate. There was no significant relationship between bile duct injury rates and annual number of procedures (P = 0.198). When only those studies that were published after 1995 were included (42 cohorts, 105570 patients) the result was similar (P = 0.19).
This systematic review examined the effect of institutional LC volume on LC outcomes-it identified 73 single centre cohorts involving 127404 patients. Using regression analyses based upon generalised estimating equations we found that there were no significant relationships between institutional LC volume and mortality (P = 0.142), bile leakage (P = 0.111) or bile duct injury (P = 0.198). However, increasing institutional LC volume was associated with reduced incidence of conversion (P = 0.019). These pooled results relate to cohorts that involved procedures performed between 1990 and 2013. Our sensitivity analysis was designed to limit the influence of the learning curve by excluding publications from before 1995-this analysis yielded similar results. Our findings are timely as mounting evidence confirms the importance of high-volume LC surgeons. Furthermore, evidence confirms the importance of high-volume centres and high-volume care providers in relation to other conditions[6]. Therefore the observation that LC complications may be influenced by institutional case load has implications for the future research and future service provision.
Our results are broadly consistent with previous studies that have examined the topic. The largest previous study was a retrospective population based study involving over one million patients from the United States National Inpatient Sample[85]. In a univariate analysis the authors of this study found that high-volume centres (≥ 225 LCs annually) had slightly improved major complication rates compared with lower-volume centres (6.4% vs 7.0%, P < 0.0001)[85]-significance was likely to have been related to the sample size and not to a clinically important effect. The effect on major complications was lost on multivariate testing. However an effect of hospital volume on conversion rates was present in a multivariable analysis-hospital volume of ≤ 120 cases per year was associated with an odds ratio (OR) for conversion of 1.32 (95%CI: 1.18-2.19) when compared with hospital volume of ≥ 225 per year. Another large population based study from Scotland involving 59918 procedures found higher mortality in lower volume (< 173 cases/year; OR = 1.45; 95%CI: 1.06-2.00; P = 0.022) and medium volume (173-244 cases/year; OR = 1.52; 95%CI: 1.11-2.08; P = 0.01) centres when high-volume centres (> 244 cases/year) were the reference group[86]. Although this again represents evidence for a hospital volume-outcome relationship for mortality, absolute effects were negligible for those patients at average risk-this suggests that the finding of significance may have simply been a reflection of the large sample size. In the late 1990s, another United States retrospective cohort study of 8602 procedures found no relationship between hospital volume and mortality[87] although a study from Norway on 4332 cases found a significant association between hospital volume and severe complications index[88]. Notably, the latter two studies only involved hospitals that nowadays would be deemed small volume.
From a wider perspective, patient safety is likely to have many underlying components and it is likely that hospital volume probably reflects clustering of these factors[86]. In the future it is important that studies explore the possibility that “high volume” may be a surrogate for streamlined management and strict adherence to protocolised care. Equivalent outcomes may be achievable in smaller centres provided that a high quality of care is maintained. High volume LC centres should only be required if institutional volume is shown to have a clinically important effect that is independent of other aspects of quality of care. As mentioned previously, several studies suggest the existence of a surgeon volume-outcome relationship for LC[2,4,5,9-12]-this seems plausible given the high-volume but low-risk nature of gallbladder surgery. The relatively low overall complication rate of gallbladder surgery makes volume-related research difficult and therefore it is essential that high quality registries including case-mix data are maintained into the future. In the long term, this will be the only way to determine important patient, surgeon and hospital-related components of safety.
The chief strength of the current study relates to the inclusion of a large number of studies, including both small and large cohorts. Furthermore, we used an extensive search strategy and we focused on patient-important outcomes that are simply defined and easily diagnosed and are thus likely to be accurate even in retrospective studies. The external validity of the study is further enhanced by the finding of average complication rates that are quite similar to accepted published rates. The main limitation is the lack of data on case mix. Furthermore, as we included studies that spanned a twenty year period across all areas of the world, undoubtedly temporal and geographical variations in care would have existed. Notably, we declined to evaluate trends in outcomes over time as study inclusion periods were heterogenous (Table 1) and results were not provided by year but rather for entire study inclusion periods. Finally we were limited to univariate analyses, thereby restricting conclusions on other factors that influence safety. We also wish to highlight that we did not aim to estimate specific optimal volume thresholds but rather we aimed to measure the effect of institutional volume on outcomes using a regression analysis. Overall, we think that the results of our review are striking. We wish to encourage research on volume-outcome relationships in surgery, particularly through the use of large scale registries.
Laparoscopic cholecystectomy (LC) is one of the most commonly performed operations worldwide. It is preferred over open cholecystectomy as it offers a shorter length of hospital stay and a quicker recovery but it is associated with the chance of needing conversion to open surgery and the risks of bile leakage, bile duct injury and mortality.
Studies have shown that institutional volume is an important determinant of outcome in a variety of conditions such as cancers, aortic aneurysms and cardiac surgery. Furthermore surgeon experience is an important factor in these conditions also. Although recent evidence suggests that surgeon volume is an important determinant of outcomes following LC, the authors have a poor understanding of the effect of institutional volume. Knowing the effect of institutional volume is important as it may influence how healthcare systems are organised.
Based on the authors review, they have identified that conversion rate is related to institutional volume. Increasing institutional LC volume leads to reduced incidence of conversion to opens surgery. The authors found no evidence to suggest the institutional volume influences mortality, bile leakage or bile duct injury rates.
Institutional volume is an important determinant of outcomes following LC. However, it is uncertain whether this is a direct effect or a surrogate for optimum standardised and protocolised care. Large scale prospective registries are needed to explore this topic further.
Bile duct injury is a serious and potentially life-threatening complication of LC resulting from inadvertent damage to biliary system structures during the operation. Bile leakage refers is a serious complication that results to continued leakage of bile from the biliary system after the operation. Most bile leaks can be managed effectively but they contribute to morbidity and have economic implications.
The current meta-analysis presents interesting.
P- Reviewer: Goetze TO, Peng B, Rabago L S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | National Centre for Health Statistics. Health, United States, 2012: With Special Feature on Emergency Care. Hyattsville, MD: National Center for Health Statistics 2013; . |
| 2. | Andrews S. Does concentration of surgical expertise improve outcomes for laparoscopic cholecystectomy? 9 year audit cycle. Surgeon. 2013;11:309-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Keus F, de Jong JA, Gooszen HG, van Laarhoven CJ. Laparoscopic versus open cholecystectomy for patients with symptomatic cholecystolithiasis. Cochrane Database Syst Rev. 2006;CD006231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 250] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 4. | Hobbs MS, Mai Q, Knuiman MW, Fletcher DR, Ridout SC. Surgeon experience and trends in intraoperative complications in laparoscopic cholecystectomy. Br J Surg. 2006;93:844-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 103] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Giger UF, Michel JM, Opitz I, Th Inderbitzin D, Kocher T, Krähenbühl L. Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J Am Coll Surg. 2006;203:723-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 220] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 6. | Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1234] [Cited by in RCA: 1226] [Article Influence: 53.3] [Reference Citation Analysis (0)] |
| 7. | Post PN, Wittenberg J, Burgers JS. Do specialized centers and specialists produce better outcomes for patients with chronic diseases than primary care generalists? A systematic review. Int J Qual Health Care. 2009;21:387-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Davoli M, Amato L, Minozzi S, Bargagli AM, Vecchi S, Perucci CA. [Volume and health outcomes: an overview of systematic reviews]. Epidemiol Prev. 2005;29:3-63. [PubMed] |
| 9. | Shi HY, Lee KT, Chiu CC, Lee HH. The volume-outcome relationship in laparoscopic cholecystectomy: a population-based study using propensity score matching. Surg Endosc. 2013;27:3139-3145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Nuzzo G, Giuliante F, Giovannini I, Ardito F, D’Acapito F, Vellone M, Murazio M, Capelli G. Bile duct injury during laparoscopic cholecystectomy: results of an Italian national survey on 56 591 cholecystectomies. Arch Surg. 2005;140:986-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 252] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 11. | Csikesz NG, Singla A, Murphy MM, Tseng JF, Shah SA. Surgeon volume metrics in laparoscopic cholecystectomy. Dig Dis Sci. 2010;55:2398-2405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 75] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 12. | McMahon AJ, Fischbacher CM, Frame SH, MacLeod MC. Impact of laparoscopic cholecystectomy: a population-based study. Lancet. 2000;356:1632-1637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 106] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264-269, W64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18463] [Cited by in RCA: 17954] [Article Influence: 1122.1] [Reference Citation Analysis (0)] |
| 14. | Szego T, Roll S, Nogueira Filho WS, Bensenor F. Videolaparoscopic cholecystectomy. Report of the first Brazilian series. Arq Gastroenterol. 1991;28:6-8. [PubMed] |
| 15. | Bailey RW, Zucker KA, Flowers JL, Scovill WA, Graham SM, Imbembo AL. Laparoscopic cholecystectomy. Experience with 375 consecutive patients. Ann Surg. 1991;214:531-540; discussion 540-541. [PubMed] |
| 16. | Peters JH, Ellison EC, Innes JT, Liss JL, Nichols KE, Lomano JM, Roby SR, Front ME, Carey LC. Safety and efficacy of laparoscopic cholecystectomy. A prospective analysis of 100 initial patients. Ann Surg. 1991;213:3-12. [PubMed] |
| 17. | Rees BI, Williams HR. Laparoscopic cholecystectomy: the first 155 patients. Ann R Coll Surg Engl. 1992;74:233-236. [PubMed] |
| 18. | Huang CS, Tai FC, Shi MY, Chen DF, Wang NY. Complications of laparoscopic cholecystectomy: an analysis of 200 cases. J Formos Med Assoc. 1992;91:785-792. [PubMed] |
| 19. | Davis CJ, Arregui ME, Nagan RF, Shaar C. Laparoscopic cholecystectomy: the St. Vincent experience. Surg Laparosc Endosc. 1992;2:64-68. [PubMed] |
| 20. | Fielding GA. Laparoscopic cholecystectomy. Aust N Z J Surg. 1992;62:181-187. [PubMed] |
| 21. | Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW. Laparoscopic cholecystectomy. The new ‘gold standard’? Arch Surg. 1992;127:917-921; discussion 921-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 298] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 22. | Périssat J, Collet D, Belliard R, Desplantez J, Magne E. Laparoscopic cholecystectomy: the state of the art. A report on 700 consecutive cases. World J Surg. 1992;16:1074-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Troidl H, Spangenberger W, Langen R, al-Jaziri A, Eypasch E, Neugebauer E, Dietrich J. Laparoscopic cholecystectomy: technical performance, safety and patient’s benefit. Endoscopy. 1992;24:252-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Rubio PA. Laparoscopic cholecystectomy: experience in 500 consecutive cases. Int Surg. 1993;78:277-279. [PubMed] |
| 25. | Huang SM, Wu CW, Hong HT, Ming-Liu KL, Lui WY. Bile duct injury and bile leakage in laparoscopic cholecystectomy. Br J Surg. 1993;80:1590-1592. [PubMed] |
| 26. | Cox MR, Wilson TG, Jeans PL, Padbury RT, Toouli J. Minimizing the risk of bile duct injury at laparoscopic cholecystectomy. World J Surg. 1994;18:422-446; discussion 426-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Williams GB, Silverman RS. Laparoscopic cholecystectomy in a community hospital: experience with 600 laparoscopic cholecystectomies. J Laparoendosc Surg. 1994;4:101-107. [PubMed] |
| 28. | Cappuccino H, Cargill S, Nguyen T. Laparoscopic cholecystectomy: 563 cases at a community teaching hospital and a review of 12,201 cases in the literature. Monmouth Medical Center Laparoscopic Cholecystectomy Group. Surg Laparosc Endosc. 1994;4:213-221. [PubMed] |
| 29. | Bonatsos G, Leandros E, Dourakis N, Birbas C, Delibaltadakis G, Golematis B. Laparoscopic cholecystectomy. Intraoperative findings and postoperative complications. Surg Endosc. 1995;9:889-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 30. | Newman CL, Wilson RA, Newman L, Eubanks S, Duncan TD, Mason EM, Wilson JP, Lucas GW. 1525 laparoscopic cholecystectomies without biliary injury: a single institution’s experience. Am Surg. 1995;61:226-228. [PubMed] |
| 31. | Chen XR, Lou D, Li SH, Mao JX, Zhou ZD, Yu SM, Duan ZW. Avoiding serious complications in laparoscopic cholecystectomy--lessons learned from an experience of 2428 cases. Ann Acad Med Singapore. 1996;25:635-639. [PubMed] |
| 32. | Bond G, De Costa A. Laparoscopic cholecystectomy: the experience of community hospital. Aust N Z J Surg. 1996;66:14-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 33. | Sartori CA, Franzato B. Laparoscopic cholecystectomy. Analysis of results of first 322 cases. Minerva Gastroenterol Dietol. 1996;42:201-205. [PubMed] |
| 34. | Rather GM, Ravi VK. Audit of laparoscopic cholecystectomies in a district general hospital. Saudi J Gastroenterol. 1997;3:15-21. [PubMed] |
| 35. | Jan YY, Chen HM, Wang CS, Chen MF. Biliary complications during and after laparoscopic cholecystectomy. Hepatogastroenterology. 1997;44:370-375. [PubMed] |
| 36. | Ahmad SA, Schuricht AL, Azurin DJ, Arroyo LR, Paskin DL, Bar AH, Kirkland ML. Complications of laparoscopic cholecystectomy: the experience of a university-affiliated teaching hospital. J Laparoendosc Adv Surg Tech A. 1997;7:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 37. | Kok KY, Mathew VV, Tan KK, Yapp SK. A prospective review of laparoscopic cholecystectomy in Brunei. Surg Laparosc Endosc. 1998;8:120-122. [PubMed] |
| 38. | Targarona EM, Marco C, Balagué C, Rodriguez J, Cugat E, Hoyuela C, Veloso E, Trias M. How, when, and why bile duct injury occurs. A comparison between open and laparoscopic cholecystectomy. Surg Endosc. 1998;12:322-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 62] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 39. | Kurauchi N, Kamii N, Kazui K, Saji Y, Uchino J. Laparoscopic cholecystectomy: a report on the community hospital experience in Hokkaido. Surg Today. 1998;28:714-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 40. | Jones-Monahan K, Gruenberg JC. Bile duct injuries during laparoscopic cholecystectomy: a community’s experience. Am Surg. 1998;64:638-642. [PubMed] |
| 41. | Matthews BD, Williams GB. Laparoscopic cholecystectomy in an academic hospital: evaluation of changes in perioperative outcomes. JSLS. 1999;3:9-17. [PubMed] |
| 42. | Calvete J, Sabater L, Camps B, Verdú A, Gomez-Portilla A, Martín J, Torrico MA, Flor B, Cassinello N, Lledó S. Bile duct injury during laparoscopic cholecystectomy: myth or reality of the learning curve? Surg Endosc. 2000;14:608-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 56] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 43. | Patel SC, Bhatt JR. Laparoscopic cholecystectomy at the Aga Khan Hospital, Nairobi. East Afr Med J. 2000;77:194-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 44. | Sikora SS, Kumar A, Das NR, Sarkari A, Saxena R, Kapoor VK. Laparoscopic bile duct injuries: spectrum at a tertiary-care center. J Laparoendosc Adv Surg Tech A. 2001;11:63-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 45. | Lichten JB, Reid JJ, Zahalsky MP, Friedman RL. Laparoscopic cholecystectomy in the new millennium. Surg Endosc. 2001;15:867-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 46. | Miroshnik M, Saafan A, Koh S, Farlow J, Neophyton J, Lizzio J, Yee F, Ethell T, Bean A, Fenton-Lee D. Biliary tract injury in laparoscopic cholecystectomy: results of a single unit. ANZ J Surg. 2002;72:867-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 47. | Hasaniah WF, Ghada I, Sabah AH, Sulaiman AH, Jamal MJ, Derar SA. Laparoscopic cholecystectomy in 2,750 cases in a teaching hospital in Kuwait. Med Princ Pract. 2002;11:176-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 48. | Fathy O, Zeid MA, Abdallah T, Fouad A, Eleinien AA, el-Hak NG, Eleibiedy G, el-Wahab MA, Sultan A, Anwar N. Laparoscopic cholecystectomy: a report on 2000 cases. Hepatogastroenterology. 2003;50:967-971. [PubMed] |
| 49. | Duca S, Bãlã O, Al-Hajjar N, Lancu C, Puia IC, Munteanu D, Graur F. Laparoscopic cholecystectomy: incidents and complications. A retrospective analysis of 9542 consecutive laparoscopic operations. HPB (Oxford). 2003;5:152-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 78] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 50. | Mahatharadol V. Bile duct injuries during laparoscopic cholecystectomy: an audit of 1522 cases. Hepatogastroenterology. 2004;51:12-14. [PubMed] |
| 51. | Daradkeh S. Laparoscopic cholecystectomy: analytical study of 1208 cases. Hepatogastroenterology. 2005;52:1011-1014. [PubMed] |
| 52. | Diamantis T, Tsigris C, Kiriakopoulos A, Papalambros E, Bramis J, Michail P, Felekouras E, Griniatsos J, Rosenberg T, Kalahanis N. Bile duct injuries associated with laparoscopic and open cholecystectomy: an 11-year experience in one institute. Surg Today. 2005;35:841-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 53. | Söderlund C, Frozanpor F, Linder S. Bile duct injuries at laparoscopic cholecystectomy: a single-institution prospective study. Acute cholecystitis indicates an increased risk. World J Surg. 2005;29:987-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 54. | Baird DR, Wilson JP, Mason EM, Duncan TD, Evans JS, Luke JP, Ruben DM, Lucas GW. An early review of 800 laparoscopic cholecystectomies at a university-affiliated community teaching hospital. Am Surg. 1992;58:206-210. [PubMed] |
| 55. | Vagenas K, Karamanakos SN, Spyropoulos C, Panagiotopoulos S, Karanikolas M, Stavropoulos M. Laparoscopic cholecystectomy: a report from a single center. World J Gastroenterol. 2006;12:3887-3890. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 56. | Tan JT, Suyapto DR, Neo EL, Leong PS. Prospective audit of laparoscopic cholecystectomy experience at a secondary referral centre in South australia. ANZ J Surg. 2006;76:335-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 57. | Mufti TS, Ahmad S, Naveed D, Akbar M, Zafar A. Laparoscopic cholecystectomy: an early experience at Ayub Teaching Hospital Abbottabad. J Ayub Med Coll Abbottabad. 2007;19:42-44. [PubMed] |
| 58. | Brekalo Z, Innocenti P, Duzel G, Liddo G, Ballone E, Simunović VJ. Ten years of laparoscopic cholecystectomy: a comparison between a developed and a less developed country. Wien Klin Wochenschr. 2007;119:722-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 59. | Marakis GN, Pavlidis TE, Ballas K, Aimoniotou E, Psarras K, Karvounaris D, Rafailidis S, Demertzidis H, Sakantamis AK. Major complications during laparoscopic cholecystectomy. Int Surg. 2007;92:142-146. [PubMed] |
| 60. | Herve J, Simoens Ch, Smets D, Ngongang Ch, Mendes da Costa P. Laparoscopic cholecystectomy; a retrospective 10-year study. Hepatogastroenterology. 2007;54:1326-1330. [PubMed] |
| 61. | Shrestha S, Pradhan G, Bhoomi K, Dhital A, Bhattachan CL. Review of laparoscopic cholecystectomy in Nepal Medical College Teaching Hospital. Nepal Med Coll J. 2007;9:32-35. [PubMed] |
| 62. | Tantia O, Jain M, Khanna S, Sen B. Iatrogenic biliary injury: 13,305 cholecystectomies experienced by a single surgical team over more than 13 years. Surg Endosc. 2008;22:1077-1086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 63. | Priego P, Ramiro C, Molina JM, Rodríguez Velasco G, Lobo E, Galindo J, Fresneda V. Results of laparoscopic cholecystectomy in a third-level university hospital after 17 years of experience. Rev Esp Enferm Dig. 2009;101:20-30. [PubMed] |
| 64. | Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C. One thousand laparoscopic cholecystectomies in a single surgical unit using the “critical view of safety” technique. J Gastrointest Surg. 2009;13:498-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 65. | Clegg-Lamptey JN, Amponsah G. Laparoscopic cholecystectomy at the Korle Bu Teaching Hospital, Accra, Ghana: an initial report. West Afr J Med. 2010;29:113-116. [PubMed] |
| 66. | Al-Kubati WR. Bile duct injuries following laparoscopic cholecystectomy: A clinical study. Saudi J Gastroenterol. 2010;16:100-104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 67. | Ying F, Shuodong W, Hong Y, Yang S, Jing K, Yu T, Amos SE. Lessons learnt after 12 years experience in laparoscopic cholecystectomy at a single center. Hepatogastroenterology. 2010;57:202-206. [PubMed] |
| 68. | Zha Y, Chen XR, Luo D, Jin Y. The prevention of major bile duct injures in laparoscopic cholecystectomy: the experience with 13,000 patients in a single center. Surg Laparosc Endosc Percutan Tech. 2010;20:378-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 69. | Wichmann MW, Lang R, Beukes E, Esufali ST, Jauch KW, Hüttl TK, Hüttl TP. Laparoscopic cholecystectomy--comparison of early postoperative results in an Australian rural centre and a German university hospital. Langenbecks Arch Surg. 2010;395:255-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 70. | Kanakala V, Borowski DW, Pellen MG, Dronamraju SS, Woodcock SA, Seymour K, Attwood SE, Horgan LF. Risk factors in laparoscopic cholecystectomy: a multivariate analysis. Int J Surg. 2011;9:318-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 71. | Al-Mulhim AS, Amin TT. Outcome of laparoscopic cholecystectomy at a secondary level of care in Saudi Arabia. Saudi J Gastroenterol. 2011;17:47-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 72. | Halilovic H, Hasukic S, Matovic E, Imamovic G. Rate of complications and conversions after laparoscopic and open cholecystectomy. Med Arh. 2011;65:336-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 73. | Hasbahceci M, Uludag M, Erol C, Ozdemir A. Laparoscopic cholecystectomy in a single, non-teaching hospital: an analysis of 1557 patients. J Laparoendosc Adv Surg Tech A. 2012;22:527-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 74. | Bekele S, Biluts H. Laparascopic cholecstectomy at Myungsung Christian Medical Center, Ethiopia: a five-years experience. Ethiop Med J. 2012;50:251-257. [PubMed] |
| 75. | Le VH, Smith DE, Johnson BL. Conversion of laparoscopic to open cholecystectomy in the current era of laparoscopic surgery. Am Surg. 2012;78:1392-1395. [PubMed] |
| 76. | Afuwape OO, Akute OO, Adebanjo AT. Preliminary experience with laparoscopic cholecystectomy in a nigerian teaching hospital. West Afr J Med. 2012;31:120-123. [PubMed] |
| 77. | Grbas H, Kunisek L, Zelić M, Petrosić N, Cepić I, Pirjavec A, Lovasić F, Uravić M. Outcome evaluation of 10,317 laparoscopic cholecystectomies: a 17-year experience at a single center. Hepatogastroenterology. 2013;60:1873-1876. [PubMed] |
| 78. | Sultan AM, El Nakeeb A, Elshehawy T, Elhemmaly M, Elhanafy E, Atef E. Risk factors for conversion during laparoscopic cholecystectomy: retrospective analysis of ten years’ experience at a single tertiary referral centre. Dig Surg. 2013;30:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 79. | Pulvirenti E, Toro A, Gagner M, Mannino M, Di Carlo I. Increased rate of cholecystectomies performed with doubtful or no indications after laparoscopy introduction: a single center experience. BMC Surg. 2013;13:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 80. | Dip FD, Asbun D, Rosales-Velderrain A, Lo Menzo E, Simpfendorfer CH, Szomstein S, Rosenthal RJ. Cost analysis and effectiveness comparing the routine use of intraoperative fluorescent cholangiography with fluoroscopic cholangiogram in patients undergoing laparoscopic cholecystectomy. Surg Endosc. 2014;28:1838-1843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 73] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 81. | Comajuncosas J, Hermoso J, Gris P, Jimeno J, Orbeal R, Vallverdú H, López Negre JL, Urgellés J, Estalella L, Parés D. Risk factors for umbilical trocar site incisional hernia in laparoscopic cholecystectomy: a prospective 3-year follow-up study. Am J Surg. 2014;207:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 82. | Paajanen H, Suuronen S, Eskelinen M, Hytonen S, Juvonen P. Frequency of bile leak after laparoscopic cholecystectomy: audit of a surgical residency program. Am Surg. 2014;80:91-94. [PubMed] |
| 83. | Alvarez FA, de Santibañes M, Palavecino M, Sánchez Clariá R, Mazza O, Arbues G, de Santibañes E, Pekolj J. Impact of routine intraoperative cholangiography during laparoscopic cholecystectomy on bile duct injury. Br J Surg. 2014;101:677-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 84. | Afaneh C, Abelson J, Rich BS, Dakin G, Zarnegar R, Barie PS, Fahey TJ, Pomp A. Obesity does not increase morbidity of laparoscopic cholecystectomy. J Surg Res. 2014;190:491-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 85. | Murphy MM, Ng SC, Simons JP, Csikesz NG, Shah SA, Tseng JF. Predictors of major complications after laparoscopic cholecystectomy: surgeon, hospital, or patient? J Am Coll Surg. 2010;211:73-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 82] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 86. | Harrison EM, O’Neill S, Meurs TS, Wong PL, Duxbury M, Paterson-Brown S, Wigmore SJ, Garden OJ. Hospital volume and patient outcomes after cholecystectomy in Scotland: retrospective, national population based study. BMJ. 2012;344:e3330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 87. | Khuri SF, Daley J, Henderson W, Hur K, Hossain M, Soybel D, Kizer KW, Aust JB, Bell RH, Chong V. Relation of surgical volume to outcome in eight common operations: results from the VA National Surgical Quality Improvement Program. Ann Surg. 1999;230:414-429; discussion 429-432. [PubMed] |
| 88. | Buanes T, Mjåland O, Waage A, Langeggen H, Holmboe J. A population-based survey of biliary surgery in Norway. Relationship between patient volume and quality of surgical treatment. Surg Endosc. 1998;12:852-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |